Specialists in Canada are concerned they could be managing a formerly obscure mind infection in the midst of a series of cases including cognitive decline, mental trips and muscle decay.
Legislators in the territory of New Brunswick have requested answers, yet with scarcely any cases, specialists say there are definitely a larger number of inquiries than answers and have asked the public not to freeze.
For over a year general wellbeing authorities have been following a “cluster” of 43 instances of suspected neurological sickness in the territory with no known reason.
Inhabitants previously scholarly of the examination a week ago after a spilled update from the territory’s general wellbeing organization requested that doctors be keeping watch for manifestations like Creutzfeldt-Jakob infection – an uncommon, lethal mind sickness brought about by misformed proteins known as prions.
“We are collaborating with different national groups and experts; however, no clear cause has been identified at this time,” said the memo.
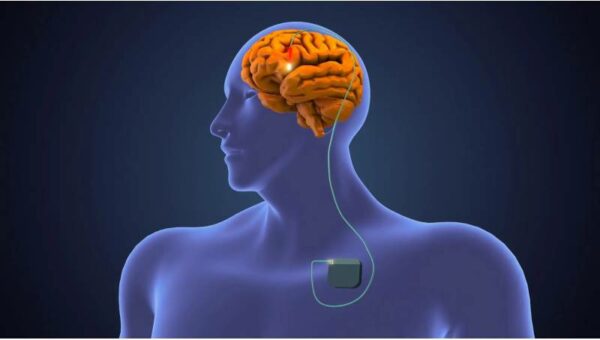
Some of the manifestations including cognitive decline, vision issues and unusual snapping developments set off a caution with Canada’s CJD observation organization. In spite of the underlying similitudes, screening delivered no affirmed instances of CJD.
“We don’t have evidence to suggest it’s a prion disease,” said Dr Alier Marrero, the nervous system specialist driving New Brunswick’s investigation.
Presently a group of specialists, including government researchers, are dashing to decide whether they are managing a formerly obscure neurological disorder, or a progression of disconnected, yet recently known – and surprisingly treatable – sicknesses.
Marrero says patients initially complained of unexplained pains, spasms and behavioural changes – all symptoms that could be easily diagnosed as anxiety or depression.
Be that as it may, more than 18 to three years they started creating psychological decay, muscle squandering, slobbering and teeth chatting. Various patients likewise started encountering alarming fantasies, including the sensation of bugs slithering on their skin.
All together for another case to be remembered for the New Brunswick “cluster”, Marrero and his group lead a broad investigation of the patient’s set of experiences, just as a battery of tests including mind imaging, metabolic and toxicology tests and spinal taps, to preclude other potential ailments like dementia, neurodegenerative problems, immune system issues and potential diseases.
Just a solitary speculated case was recorded in 2015, yet in 2019 there were 11 cases and 24 of every 2020. Analysts accept five individuals have kicked the bucket from the sickness.
“We have not seen over the last 20-plus years a cluster of diagnosis-resistant neurological disease like this one,” said Michael Coulthart, head of Canada’s CJD surveillance network.
Most of cases are connected to the Acadian landmass, a meagerly populated locale in the north-eastern piece of the area. The general number of cases in the bunch stays low yet New Brunswick has a populace of less than 800,000 individuals.
Wellbeing authorities have would not unveil the exact areas of the cases.
Marrero and his group have counseled specialists in nervous system science, natural wellbeing, field the study of disease transmission, zoonotics and toxicology to all the more likely comprehend what could be causing the secret sickness.
A developing group of analysts is attempting to decide whether there is a typical connect to the cases or any natural causes, including water sources, plants and bugs.
Cautioning of genuine mind problems in individuals with gentle Covid side effects
Understand more
“We don’t have a clue what is causing it,” said Marrero. “Right now we just have more patients seeming to have this syndrome.”
Information on the obscure disease has provoked concern yet specialists have forewarned against making untimely inferences.
“I don’t really know if we even have a defined syndrome. There just isn’t enough information yet,” said Valerie Sim, a scientist of neurodegenerative sicknesses at the University of Alberta.
She noticed that vital markers for degenerative neurological ailments had not been recorded and that the wide scope of indications in the bunch was “atypical” for most mind infections. Simultaneously, certain tumors, dementia or even misdiagnoses could clarify the extent of indications, she said.
The adventure additionally uncovered the baffling truth of medication: diagnosing a patient can be intense and it is an undertaking filled with questions. Nervous system specialists can regularly convey various apparatuses in treating a patient when the underlying driver of an infirmity is hazy, “and then the patient somehow recovers. You come away never knowing what they actually had,” said Sim.
“We see odd neurological syndromes from time to time. Sometimes we figure them out. Sometimes we don’t.”