A recent clinical experiment demonstrates that severe to moderate depression can be safely and efficiently treated with at-home brain stimulation therapy.
The noninvasive brain stimulation was associated with three times greater rates of therapy response and depression remission, according to the researchers.
As the chair of psychiatry at the University of Texas McGovern Medical School, co-lead researcher Dr. Jaire Soares remarked, “The study results bring promise that an innovative treatment modality may become available for patients suffering from mood disorders some time in the near future.”
In the trial, 174 individuals with a diagnosis of depression were randomized to either receive or not receive brain stimulation during the course of ten weeks of treatment.
For the first three weeks, participants in the brain stimulation program received five 30-minute sessions per week; for the next seven weeks, they received three 30-minute sessions each week.
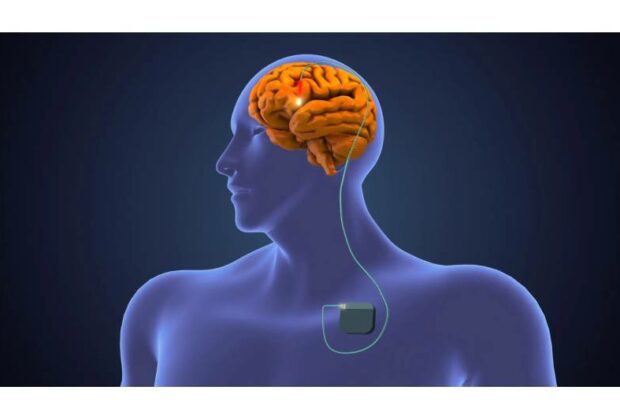
Transcranial direct current stimulation (tDCS) is the name of the treatment, which involves applying a current of 0.5–2 milliamperes to the head via two electrodes. The maximum effect of this quantity of electricity is a mild tingling feeling along the scalp.
According to the researchers, patients self-administered the stimulation in their homes.
Researchers discovered that almost 45% of those who received the stimulation ended up with their depression in remission, compared to 22% of the control group.
“The burden of depression is mostly keenly felt by the 280 million people worldwide currently managing symptoms. While a combination of antidepressants and therapy generally proves to be effective for many people, medication can have side effects that some can find disruptive,” According to lead researcher Dr. Cynthia Fu, a professor of affective neuroscience and psychotherapy at King’s College London.
As stated in a news release from the University of Texas, “Our study has demonstrated that tDCS is a potential first-line option that could help those in need,” Fu continued.
The stimulation device’s maker, Flow Neuroscience, provided funding for the study.