During National Health IT Week, three specialists put the attention on how computerized advances and keen consideration methodologies are as of now changing populace wellbeing and helping address social determinants.
As a component of its National Health IT Week program, HIMSS introduced an online class this week investigating the appearance of what it calls the “Smart Communities-Cities Movement.”
Medicinal services all of a sudden winds up in the midst of a change in outlook, where a bounty of ongoing clinical and social wellbeing information, broadband network, individual gadgets, sensors, applications, advanced therapeutics and more are changing conveyance away from intense consideration settings and into the bigger network.
It’s a principal change that is just going to be progressively articulated in the years ahead as the requests of commercialization and worth based consideration, joined with continuous advances in consistently on innovation, keep up the energy toward new models of consideration.
“How healthcare is organized will be drastically different because of technology,” said Dr. Chris Gibbons, author and CEO of The Greystone Group, during the HIMSS session – which is currently on-request and investigates how suppliers and government, state and neighborhood policymakers are changing the manner in which they consider the web of things and associated wellbeing apparatuses as they center around populace wellbeing the board.
The commonness (if not universality) of broadband, joined with quick propelling apply autonomy, ingestible advancements and wearable sensors as slight and lightweight as brief tattoos – to give some examples late developments – are set to change “medical services, public health, social services. wellness” and the sky is the limit from there, said Gibbons — to avoid anything related to totally reshaping the patient experience.
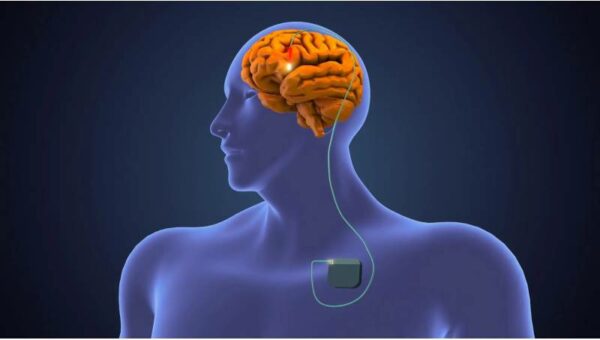
Savvy innovation –”embedded chips that can detect automatically and react appropriately without human interaction,” or digital health tools that “have the processing power embedded right in them” – are now making their essence felt.
Also, as these AI-empowered IoT systems multiply crosswise over networks and whole urban communities, the outcome will be “real-time delivery of automated health services, anywhere the person is located in the community,” said Gibbons.
In this not so distant future, “there is no place these people are not connected,” they clarified. “They do not need to be in a hospital. You can really envision the delivery of automated services – public health services, social services – anywhere to the person in the community.
“Digital technologies and smart care approaches will transform healthcare organizations far beyond the practice of medicine, yet they will also provide significant opportunities to improve population health,” they added.
Also, just in time, said Dr. Asif Dhar, boss wellbeing informatics official at Deloitte.
The primary drivers of expense in the U.S. – and they are cosmic expenses – are for ceaseless sickness and fixation: medical problems that exist outside of the clinic setting and along these lines should be handled in the network on the loose.
The U.S. burned through $327 billion on diabetes the executives in 2017, Dhar said. The all out spending on enslavement, and all its auxiliary expenses, is probably going to surpass $740 billion. These monstrous uses on conduct based ailment could be stayed away from, to avoid anything related to the genuine human cost: “more than 42 percent of cancers are deemed to be preventable if we had different behaviors.”
The foundation of an online wellbeing network around a particular medical problem (weight reduction, for instance), scaled up by sending custom applications, consolidating gamification and “nudging” for inspiration and joining “digital sidewalks” for virtual network gatherings, are one route forward.
“Communities are major players in the future of healthcare,” they said. “The coming together of exponential technologies, behavioral science, biology and clinical medicine in order to develop and shape communities, hubs and conditions (will) dramatically reduce costs and improve wellness and longevity.”
These savvy wellbeing networks ought to have five key components, Dhar clarified. They should 1) engage proactive wellbeing and prosperity the board; 2) cultivate a feeling of network and prosperity; 3) be empowered by advanced innovation and social science; 4) genuinely use information to improve results; 5) empower new, imaginative biological systems.
Leave it to a spot like Portland, Oregon, to as of now be displaying what these new environments can resemble.
Skip Newberry, president and CEO of the Technology Association of Oregon, has been managing some interesting advancements in associated wellbeing there, attempting to build up a “culture of consumer success” – he supports that to the expression “consumerization,” since it has a few undertones that make some human services partners bristle – empowered by broadly scattered innovations over the city.
Activities, for example, Smart City PDX, for instance, are sending driving edge innovations to support its residents, particularly underserved networks.
It begins with little pilots, gains from them, and after that scales up. It uses existing spending cash to look after supportability.
Among its tasks are an open information program, a urban information lake, air quality sensor organizations and sunlight based controlled brilliant stands for fiasco readiness called PREPHubs, intended to work off-network while offering force, correspondence and medical aid supplies.
The point, said Newberry, is to “take the built environment and make it more connected: device to device, and also human to device.”
Up until now, one key zone of advancement has been on social determinants of wellbeing, for example, vagrancy and nourishment security: “One thing we’ve been focused on is trying to bridge the gap between government, community organizations and residents,” they said.